Section: Research Program
Real Time Patient-Specific Computational Models
Accounting for the biomechanics and physiology of organs under various stimuli requires employment of biomechanical models. These must describe biophysical phenomena such as soft-tissue deformation, fluid dynamics, electrical propagation, or heat transfer. We aim at simulating the impact of certain therapies (such as cryosurgery or radio-frequency ablation) and representing the behavior of complex organs such as the brain, the liver or the heart.
An important part of our research is dedicated to the development of new accurate models that remain compatible with real-time computation [6]. Such advanced models do not only permit to increase the realism of future training systems, but they act as a bridge toward the development of patient-specific preoperative planning as well as augmented reality tools for the operating room [5] [40], [54]. Yet, patient-specific planning or per-operative guidance also requires the models to be parametrized with patient-specific biomechanical data. Our objective is the study of hyper-elastic models and their validation for a range of tissues. Preliminary work has been done through two collaborations, one with the biomechanical lab in Lille (LML) [42], and the biomechanics group from the Icube laboratory in Strasbourg on the development and validation of liver and kidney models [52].
Another important research topic is related to model reduction through various approaches, such as Proper Generalized Decomposition (PGD) [35]. Similar approaches, such as the use of Krylov spaces, have already been studied in our group recently [33].
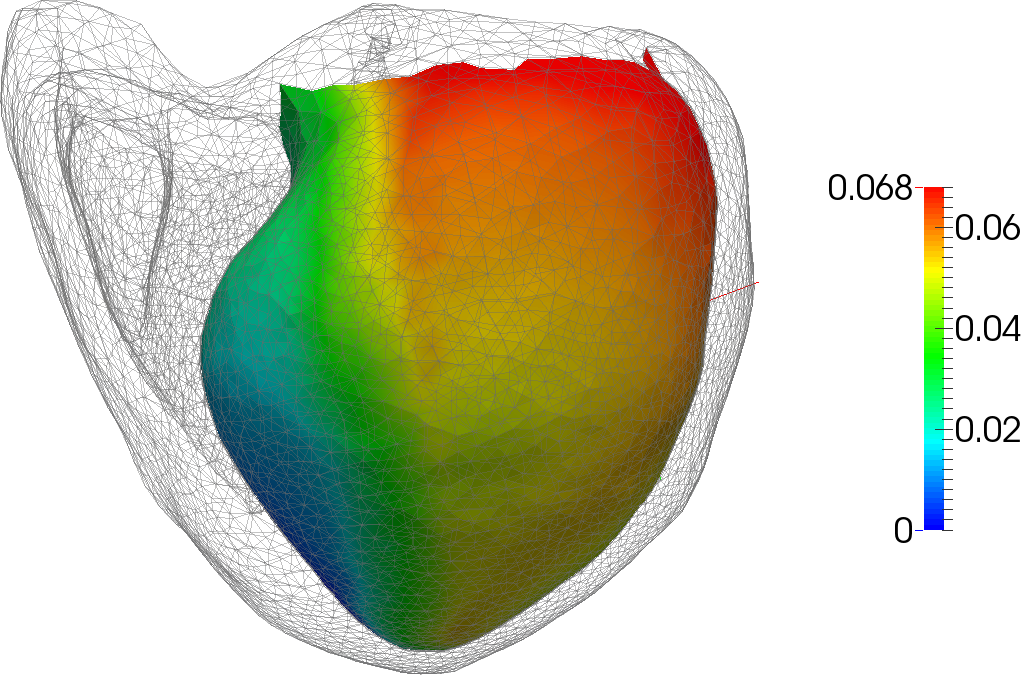
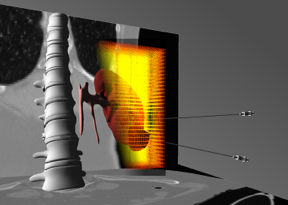
We continue our work on cardiac electro-physiology simulation [53], with a focus on patient-specific adaptation of the model. We also study a similar problem, related to the modeling of the electrical conduction in the brain, in the context of Deep Brain Stimulation (DBS) [34], [38]. In this neurosurgical procedure, electrodes are implanted deep into the brain and, connected to a brain pacemaker, send electrical impulses to specific regions. A final objective is to solve optimization problems in the context of heat diffusion. This is a key element of the development of a planning system that can estimate the locations of the electrodes leading to an optimal therapeutic effect [54].