Section: Research Program
Image-Driven Simulation
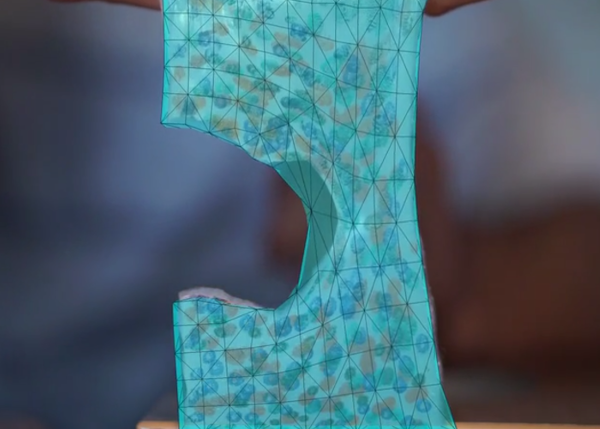
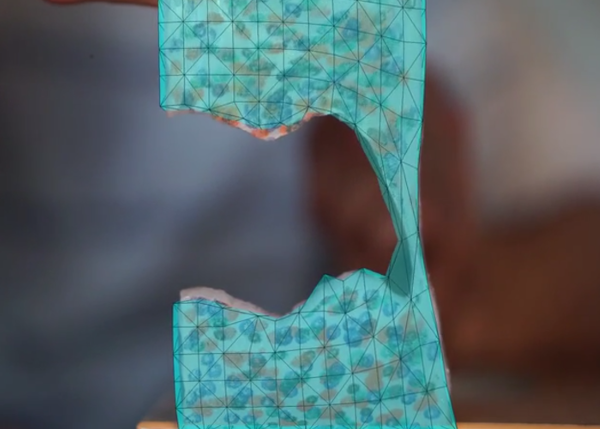
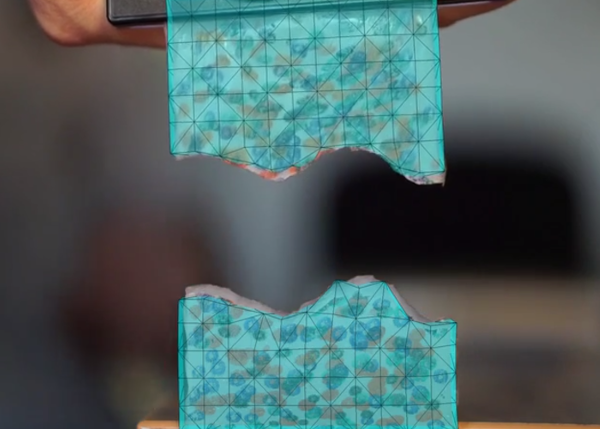
Image-guided simulation is a recent area of research that has the potential to bridge the gap between medical imaging and clinical routine by adapting pre-operative data to the time of the procedure. Several challenges are related to image-guided therapy but the main issue consists in aligning pre-operative images onto patient per-operative data and keep this alignment up-to-date during the procedure. As most procedures deal with soft-tissues, elastic registration techniques are necessary to perform this step. Recently, registration techniques started to account for soft tissue biomechanics using physically-based methods, yet several limitations still hinder the use of image-guided therapy in clinical routine. First, as registration methods become more complex, their computation times increase, thus lacking responsiveness. Second, techniques used for non-rigid registration or deformable augmented reality only “borrow” ideas from continuum mechanics but lack some key elements (such as identification of the rest shape, or definition of the boundary conditions). Also, these registration or augmented reality problems are highly dependent on the choice of image modality and require investigating some aspects of computer vision or medical image processing. However, if we can properly address these challenges, the combination of a real-time simulation and regular acquisitions of image data during the procedure opens up very interesting possibilities by using data assimilation to better adapt the model to the intra-operative data. In the area of non-rigid registration and augmented reality, we have already demonstrated the benefit of our physics-based approaches. This was applied in particular to the problem of organ tracking during surgery (Figure 5 ) and led to several key publications [35] , [36] , [34] and awards (best paper at ISMAR 2013, second best paper at IPCAI 2014). We continued this work with an emphasis on robustness to uncertainty and outliers in the information extracted in real-time from image data. We also improved our computer vision techniques, in particular to guarantee a very accurate initial registration of the pre-operative model onto the per-operative surface patch extracted from monocular or stereo laparoscopic cameras.
|
The use of simulation in the context of image-guided therapy can be extended in several other ways. A direction we particularly want to address is the combined use of simulation and X-ray imaging during interventional radiology procedures. Whether it is for percutaneous procedures or catheterization, the task of the simulation is to provide a short-term (1 to 5 seconds) prediction of the needle or catheter position. Using information extracted from the image, the parameters of the simulation can be assimilated (using methods such as unscented Kalman filters), so that the simulation progressively matches the real data in order to reduce uncertainties. We have already started to create a flexible framework integrating the real-time soft-tissue simulation and state-of-the-art methods of data assimilation and filtering. The reduced-order stochastic filtering is a computationally efficient improvement over traditional computationally expensive approaches which fits well the real-time and patient-specific requirements arising from our per-operative context.